Key Takeaways
- Definition: Medical PCB assembly goes beyond standard electronics manufacturing by strictly adhering to ISO 13485 standards and IPC Class 3 reliability requirements.
- Critical Metrics: Success is measured by First Pass Yield (FPY), ionic cleanliness levels, and complete component traceability down to the lot number.
- Misconception: Many assume all medical boards require the most expensive materials, but material selection should actually depend on the specific device classification (Class I, II, or III).
- Pro Tip: Early involvement in Design for Manufacturing (DFM) can reduce validation costs by up to 30% by catching footprint errors before the first prototype.
- Validation: A robust testing strategy must combine Automated Optical Inspection (AOI), X-Ray, and In-Circuit Testing (ICT) to ensure zero defects in life-critical applications.
- Traceability: Every component on the Bill of Materials (BOM) must be traceable to its source to facilitate rapid recalls or investigations if field failures occur.
What medical pcb assembly really means (scope & boundaries)
Medical PCB assembly is the specialized process of fabricating and populating printed circuit boards used in healthcare devices, ranging from diagnostic equipment to life-sustaining implants. Unlike consumer electronics, where cost is often the primary driver, medical electronics prioritize patient safety, reliability, and regulatory compliance.
At APTPCB (APTPCB PCB Factory), we define this scope through three critical boundaries: regulatory adherence, reliability classification, and lifecycle management.
First, regulatory adherence centers on ISO 13485. This is the quality management system standard specifically for medical devices. It requires documented procedures for every step of the assembly process, ensuring that every board produced is identical to the validated design.
Second, reliability is governed by IPC classification. Most medical devices fall under IPC Class 2 (Dedicated Service Electronic Products) or IPC Class 3 (High Reliability Electronic Products). Class 3 is mandatory for life-support systems where downtime is not an option. This dictates stricter criteria for solder joint quality, plating thickness, and cleanliness.
Third, lifecycle management involves strict change control. In medical manufacturing, you cannot simply swap a capacitor for a cheaper alternative without validating that the change does not impact clinical performance. This rigorous control ensures that the device approved by the FDA or CE remains the device being manufactured years later.
Metrics that matter (how to evaluate quality)
Once you understand the scope, you need specific data points to measure success and ensure the assembly meets medical standards.
In medical electronics, "good enough" does not exist. You must quantify quality using metrics that reflect both the manufacturing process health and the final product reliability.
| Metric | Why it matters | Typical range or influencing factors | How to measure |
|---|---|---|---|
| First Pass Yield (FPY) | Indicates process stability. Low FPY suggests systemic issues that could lead to latent field failures. | >98% for mature medical products; >95% for complex mixed-technology boards. | (Good units / Total units entering process) × 100. |
| Ionic Contamination | Residues can cause dendritic growth and shorts, especially in humid hospital environments or implants. | <1.56 µg/cm² NaCl equivalent (standard); <0.75 µg/cm² for high-reliability. | ROSE testing (Resistivity of Solvent Extract) or Ion Chromatography. |
| Solder Void Percentage | Voids in solder joints reduce thermal and mechanical performance, critical for power components and BGAs. | IPC Class 3 allows max 25% voiding area; <10% is preferred for medical. | 2D or 3D X-Ray inspection analysis. |
| Component Traceability | Essential for recalls. You must know which batch of capacitors went into which serial number. | 100% coverage. Must link Ref Des to Manufacturer Lot Number. | ERP/MES systems scanning reels during placement. |
| Test Coverage | Ensures that the manufacturing defects are actually detectable before shipping. | >95% coverage of potential defects (shorts, opens, wrong values). | Combined analysis of AOI, X-Ray, ICT, and Functional Test capabilities. |
| Thermal Cycle Survival | Predicts lifespan under stress (e.g., sterilization cycles or varying operating temps). | -40°C to +85°C (or wider depending on use case) for 500+ cycles. | Accelerated Life Testing (ALT) chambers. |
Selection guidance by scenario (trade-offs)
Knowing the metrics helps, but different medical devices require different manufacturing priorities based on their clinical application.
Not all medical PCBs are created equal. A disposable diagnostic tool has vastly different requirements than a pacemaker. Here is how to balance trade-offs across common scenarios.
1. Implantable Devices (Pacemakers, Neurostimulators)
- Priority: Extreme miniaturization and absolute reliability (IPC Class 3).
- Trade-off: High cost and low yield tolerance vs. longevity.
- Key Requirement: Use of biocompatible materials and high-reliability substrates like polyimide flex.
- APTPCB Insight: Cleanliness is paramount here; any ionic residue can cause failure inside the body.
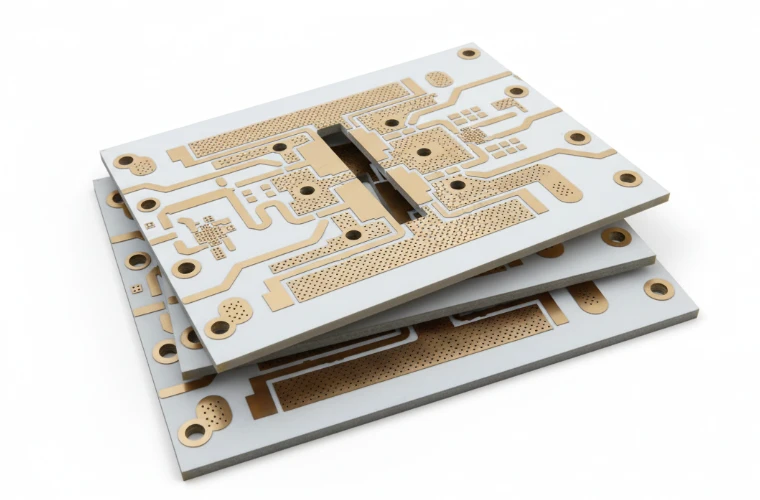
2. Diagnostic Imaging (MRI, CT, Ultrasound)
- Priority: Signal integrity and high-speed data processing.
- Trade-off: Complex layer stacks (12+ layers) vs. manufacturability.
- Key Requirement: Controlled impedance and low-loss materials.
- Recommendation: Utilize Rogers PCB materials to minimize signal loss at high frequencies.
3. Wearable Health Monitors (ECG patches, Glucose monitors)
- Priority: Form factor (flexibility) and power consumption.
- Trade-off: Durability vs. comfort/weight.
- Key Requirement: Rigid-flex construction to fit curved enclosures.
- Risk: Dynamic flexing can crack solder joints if the bend radius is too tight.
4. Surgical Robotics
- Priority: Precision motor control and low latency.
- Trade-off: Thermal management vs. component density.
- Key Requirement: Heavy copper PCBs to handle high currents for motors without overheating.
- Validation: Extensive vibration testing is required to simulate the operating environment.
5. Laboratory Instrumentation (Blood Analyzers)
- Priority: Chemical resistance and long-term stability.
- Trade-off: Robustness vs. aesthetic design.
- Key Requirement: Conformal coating to protect against chemical spills and reagents.
- Focus: High mix, low volume production is common here.
6. Home Health Equipment (CPAP, Nebulizers)
- Priority: Cost-effectiveness and user safety (insulation).
- Trade-off: Consumer-grade pricing vs. medical-grade safety.
- Key Requirement: Strict adherence to UL safety standards for flammability and electric shock.
- Strategy: Use standard FR4 materials but maintain strict process controls.
From design to manufacturing (implementation checkpoints)
After selecting the right approach for your scenario, the focus shifts to the step-by-step execution of the assembly process.
This phase is where the theoretical design meets the physical reality of manufacturing. We recommend the following checkpoints to ensure your medical pcb assembly runs smoothly.
Checkpoint 1: Material Verification
- Recommendation: Verify that the laminate (FR4, Rogers, Flex) matches the UL file and flammability rating specified.
- Risk: Using non-certified materials can void FDA 510(k) submissions.
- Acceptance: Certificate of Conformance (CoC) from the laminate supplier.
Checkpoint 2: Design for Manufacturing (DFM) Review
- Recommendation: Run a comprehensive DFM check before ordering stencils.
- Risk: Pad sizes that are too small for Class 3 annular rings will cause breakout.
- Acceptance: Approval of the DFM report. You can use DFM guidelines to prepare.
Checkpoint 3: Solder Paste Printing
- Recommendation: Use electroformed stencils for fine-pitch components (0201, BGA).
- Risk: Insufficient paste leads to open joints; too much leads to bridging.
- Acceptance: 3D Solder Paste Inspection (SPI) volume data.
Checkpoint 4: Component Placement
- Recommendation: Verify feeder setup to ensure the correct MPN (Manufacturer Part Number) is loaded.
- Risk: Wrong capacitor voltage rating can lead to catastrophic failure.
- Acceptance: Machine verification logs and First Article Inspection (FAI).
Checkpoint 5: Reflow Profiling & BGA Control
- Recommendation: Optimize the thermal profile to minimize voiding in Ball Grid Arrays (BGAs).
- LSI Focus: bga voiding control: stencil, reflow, and x-ray criteria.
- Stencil: Aperture design should be reduced (e.g., 70-80% of pad) to prevent excess flux gas entrapment.
- Reflow: A soak zone allows volatiles to escape before the alloy melts.
- Criteria: IPC Class 3 demands strict limits on void size (typically <25% of ball area).
- Acceptance: Thermal profile graph within spec.
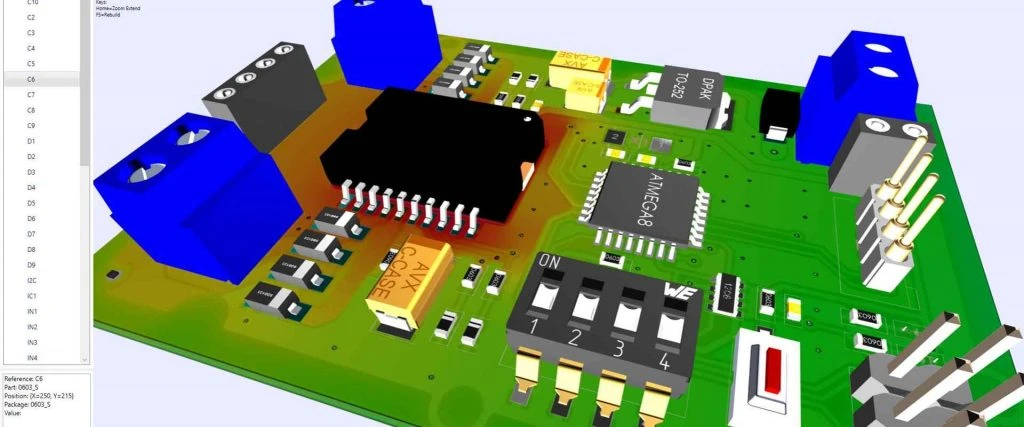
Checkpoint 6: Automated Optical Inspection (AOI)
- Recommendation: Deploy AOI after reflow for all boards.
- LSI Focus: aoi vs x-ray inspection: what defects each catches.
- AOI: Best for visible defects like polarity, tombstoning, bridging, and missing parts. It relies on light reflection and cameras.
- X-Ray: Essential for hidden joints (BGA, QFN, LGA). It detects voiding, shorts under the package, and head-in-pillow defects that AOI cannot see.
- Acceptance: Zero false passes; verified by human operator.
Checkpoint 7: In-Circuit Testing (ICT) / Flying Probe
- Recommendation: Perform electrical testing to verify component values and detect shorts/opens.
- Risk: Passive components with the wrong value but correct package size are invisible to AOI.
- Acceptance: Pass/Fail log for every serial number.
Checkpoint 8: Cleaning and Conformal Coating
- Recommendation: Wash boards to remove flux residues, then apply coating if required for moisture protection.
- Risk: Ionic residue causes corrosion over time.
- Acceptance: Ionic contamination test results.
Common mistakes (and the correct approach)
Even with a solid plan, specific pitfalls can derail a medical electronics project if not anticipated.
These mistakes often stem from treating medical boards like consumer electronics. Avoiding them saves time and regulatory headaches.
Ignoring Component Obsolescence:
- Mistake: Designing with parts that are Near End of Life (EOL).
- Correction: Check the lifecycle status of every component. Medical products have long lifecycles (5-10 years), so select parts with guaranteed long-term availability.
Insufficient Test Points:
- Mistake: Removing test points to save space, making ICT impossible.
- Correction: Prioritize testability. If physical test points don't fit, plan for extensive boundary scan (JTAG) or functional testing fixtures.
Ambiguous Documentation:
- Mistake: Sending Gerbers without a fabrication drawing or assembly notes.
- Correction: Provide a complete package including stackup, drill chart, IPC class requirement, and color of soldermask/silkscreen.
Neglecting Sterilization Effects:
- Mistake: Choosing materials that degrade under Gamma, EtO, or Autoclave sterilization.
- Correction: Verify that the PCB substrate, soldermask, and components can withstand the intended sterilization method of the final device.
Over-specifying Tolerances:
- Mistake: Requiring +/- 1% impedance on traces where +/- 10% is sufficient.
- Correction: Tight tolerances increase cost and scrap. Use an impedance calculator to determine realistic parameters.
Late Supplier Engagement:
- Mistake: Finishing the design before talking to the manufacturer.
- Correction: Engage APTPCB early. We can suggest stackup optimizations that improve yield without changing signal performance.
FAQ
To clarify any remaining uncertainties, here are answers to the most frequent questions we receive regarding medical assembly.
Q: What is the difference between ISO 9001 and ISO 13485? A: ISO 9001 is a general quality management standard. ISO 13485 is specific to medical devices, adding strict requirements for risk management, documentation, and traceability that ISO 9001 does not cover.
Q: Can medical PCBs use lead-free solder? A: Yes, most medical devices now comply with RoHS (lead-free). However, some critical life-support categories still have exemptions allowing leaded solder to prevent tin whiskers, though this is becoming rarer.
Q: How do you handle firmware programming? A: We can pre-program ICs before placement or program them on-board using a test fixture. We require a checksum verification to ensure the code is loaded correctly.
Q: What is the typical lead time for medical PCB assembly? A: Prototypes can be done in 24-72 hours. Production runs typically take 2-4 weeks, depending on component lead times and the complexity of testing required.
Q: Do you support rigid-flex for medical wearables? A: Yes, rigid-flex is very common in medical wearables. We support complex stackups to allow the device to conform to the patient's body.
Q: How is confidentiality handled? A: We sign a Non-Disclosure Agreement (NDA) before receiving any data. Your IP is protected throughout the manufacturing process.
Q: What happens if a component is out of stock? A: We propose alternates with identical form, fit, and function. However, in medical assembly, you (the customer) must approve any alternate before we proceed.
Q: Is X-Ray inspection mandatory? A: For boards with BGAs, LGAs, or QFNs (leadless parts), X-Ray is mandatory to ensure solder joint quality. For boards with only visible leads, AOI is usually sufficient.
Related pages & tools
For deeper technical analysis and to prepare your data for production, utilize these specific resources.
- DFM Guidelines: Detailed design rules to ensure your board is manufacturable.
- SMT & THT assembly: Core assembly process overview for medical boards with mixed SMT/THT content.
- Impedance Calculator: Calculate trace width and spacing for controlled impedance lines.
- Get a Quote: Submit your files for a detailed cost estimation.
Glossary (key terms)
Finally, ensure clear communication by reviewing standard industry terminology used in medical electronics manufacturing.
| Term | Definition |
|---|---|
| IPC-A-610 Class 3 | The highest standard for electronic assembly acceptance, required for high-reliability and life-support medical devices. |
| ISO 13485 | The international quality management standard specifically for the medical device industry. |
| BOM (Bill of Materials) | A comprehensive list of all components, including MPNs, quantities, and reference designators. |
| Gerber Files | The standard file format used to convey PCB layer data (copper, soldermask, drill) to the manufacturer. |
| Fiducial Marker | A copper mark on the PCB used by assembly machines for optical alignment. |
| Reflow Soldering | A process where solder paste is melted in an oven to attach surface mount components. |
| Wave Soldering | A process used primarily for through-hole components where the board passes over a wave of molten solder. |
| SMT (Surface Mount Technology) | A method where components are mounted directly onto the surface of the PCB. |
| AOI (Automated Optical Inspection) | A camera-based system that scans the PCB for visual defects like missing parts or polarity errors. |
| AXI (Automated X-Ray Inspection) | An inspection method using X-rays to see solder joints hidden under components like BGAs. |
| ICT (In-Circuit Test) | A test method that uses a "bed of nails" fixture to check the electrical integrity of individual components. |
| Conformal Coating | A protective chemical layer applied to the PCB to guard against moisture, dust, and chemicals. |
| Traceability | The ability to track the history, application, or location of an item (component) by means of recorded identification. |
Conclusion (next steps)
Summarizing the journey from definition to validation ensures your project is ready for the market.
Medical PCB assembly is a discipline that tolerates no errors. It requires a synergy between robust design, precise material selection, and a manufacturing partner who understands the gravity of IPC Class 3 standards. From controlling BGA voiding to ensuring complete traceability, every step protects the end patient.
To move forward, prepare your data package—including Gerber files, BOM, assembly drawings, and test requirements. At APTPCB, we are ready to review your documentation and guide you through the transition from prototype to volume production.
Ready to validate your medical design? Contact us today for a comprehensive DFM review.